CAUDA EQUINA AND CONUS INJURIES
OVERVIEW
Injuries to the nerves at the bottom or just below the spinal cord have similarities and differences from spinal cord injury. This chapter briefly describes cauda equina syndrome and conus injuries, how they are different from injuries higher up on the spinal cord and how these injuries affect daily life.
- Introduction
- What are the conus and cauda equina?
- What Do I Need to Know?
- Injury classification
- What’s Different Now?
- Prognosis
- What Can I Do?
- Bowel and bladder management
- Skin care
- Pain management
- Muscle Imbalances
- Rehabilitation
- Who Can Help Me?
- Conclusion & Resources
INTRODUCTION
What are the conus and cauda equina?
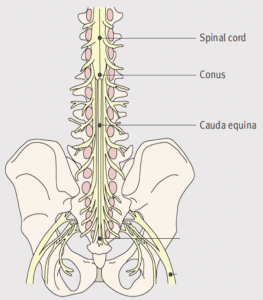
Posterior cross section of the lower spine, sacrum and pelvis, showing the conus and cauda equina, parts of the central nervous system affected by cauda equina syndrome or a conus injury.
A person’s spinal cord is shorter than the column of bones in the spine (called vertebrae), ending somewhere between the 12th thoracic (T12) vertebrae and the 2nd Lumbar (L2) vertebrae.
The place where the spinal cord ends is shaped like a cone, and is called the conus.
The upper motor neurons (also known as central motor neurons), long nerve cells which run from the brain to the spinal cord, end at the conus. There, they meet and send information to the lower motor neurons (also known as peripheral motor neurons), which run from the spinal cord to the lower body.
DID YOU KNOW?
WHAT DO I NEED TO KNOW?
Injury classification is difficult!
- Sometimes a cauda equina injury is said to not be a “true” spinal cord injury because they affect the peripheral nerves very close to, but not part of, the spinal cord. Peripheral and central neurons respond differently to injury and don’t easily fit our injury classification systems (as mentioned below). This distinction is meaningful to healthcare providers in terms of understanding your recovery and rehabilitation, but your injury is just as real.
- For this reason, the ASIA classification (see understanding SCI), which does try to classify these injuries, can be very confusing – you might be able to use your legs, but be classified as an “ASIA A”, which is a motor and sensory complete injury.
- Try not to get too hung up on ASIA classification, because it’s just a letter – it doesn’t describe you or your injury. Talk to your healthcare team if you want more details.
WHAT’S DIFFERENT NOW?
How will my signs and symptoms be different than other spinal cord injuries?
Injury to the upper motor nerves and lower motor nerves cause different signs and symptoms. Generally, lower motor neuron (including cauda equina) injuries affect the body in a well recognized pattern:
- The bladder, bowel and sexual function are the most affected in people with these types of injuries, in different ways than seen in upper motor neuron injuries.
- “Flaccid” bowel and bladder – these are patterns of bowel and bladder dysfunction that tend to be caused by low or poor muscle tone, and difficulty with complete emptying, such as urinating or emptying the bowel continuously or without warning unless a careful routine is used. Read more about flaccid bladder and bowel.
- Sexual changes (for more on this visit SCISexualHealth.ca)
- Decreased reflexes
- Very few or no spasms
- Loss of more muscle bulk compared with other injuries
- Increased flexibility
- Less response to electrical muscle stimulation for strengthening
- Increased numbness and nerve pain in the pelvis and groin
Injuries to the conus (between thoracic 12 and Lumbar 2), are sometimes called “mixed” injuries, meaning that you can have symptoms of both upper motor neuron and lower motor neuron injuries. This can be very frustrating because you don’t fit into either category, and it may be unclear at first which bladder and bowel tools and routines will work for you.
Prognosis
- Like other spinal cord injuries, how much function you will recover after a conus or cauda equina injury and how quickly this will happen is difficult to predict.
- Lower motor nerves and sensory nerves have more potential for regrowth than upper motor nerves, but the growth is very slow. It is thought that the timeline for recovery in these injuries is longer. What your signs and symptoms might look like during rehab can be very different than a few years later.
WHAT CAN I DO?
Manage your bowel and bladder – don’t let them manage you
You are more likely to have accidents than someone with an upper motor neuron injury, which can be embarrassing and frustrating. Review the bowel and bladder management chapters in this resource and don’t give up!
Take care of your skin
With lost muscle bulk, the bones in your bottom protrude more; with decreased sensation, you may not feel when the skin breaks down. Even though you might be able to move more easily than people with other injuries, pressure relieving equipment and strategies are very important.
Learn about and manage your pain.
Pelvic and groin pain can be very debilitating, so figure out what techniques work for you. See our chapter on Pain.
Watch for muscle imbalances.
A common issue seen in these types of injuries is that some muscles (usually in the front of the leg) work very well, while others don’t work at all (usually in the back of the leg). This is called a muscle imbalance. It’s important to work with your healthcare team to protect your joints, because muscle imbalances can cause pain and arthritis long term.
Maximize your learning in rehabilitation.
You’ll have the most nursing care and therapy while you’re in rehab so use the time to ask questions and connect with clinicians and peers who can help when you need it, even after you return home.
Understand that your rehabilitation doesn’t stop when you leave rehab.
The road to your maximum recovery may be a bit longer with these injuries than in other spinal cord injuries.
Understand that people may not understand your injury.
Some people with these injuries are called the “walking wounded” because their symptoms or functional changes are less visible, and they are able to walk or move in ways that most people wouldn’t expect after an injury to the spine. Remember that their misunderstanding of your injury does not change the reality of the injury or its effect on your life.
Become the best expert you can be on your condition.
It’s important to learn and practice explaining your condition and how it affects you to those around you, including to healthcare providers – conus and cauda equina injuries are very individual, so you will be the best expert on how it affects you. Learning to explain it in a simple and confident way will be very helpful in getting help, support or knowing what is normal for you now.
WHO CAN HELP ME?
All clients/patients have a team of healthcare professionals working with them – there are so many at times it can be very confusing! Take the time to find out who they are and what they do.
Your team may consist of one or several of the following types of healthcare professionals, all aimed at supporting a different aspect of your recovery and rehabilitation. In many cases, you may see different people in the same role depending on the shift, time of week or their area of expertise. In addition, teaching hospitals like Vancouver General Hospital and GF Strong Rehab Centre also have medical and nursing trainees on staff who assist in care as part of their training.
Nursing Staff
Social Work (SW)
The role of a social worker is to provide emotional support and practical assistance to the patient and their family. They are there to support people through the various concerns that arise from a serious illness or injury, provide crisis intervention, and can assist patients to access community and government resources. Social workers also help patients navigate the healthcare system, connect with other professionals, arrange family meetings, and assist with discharge planning.
Physiotherapist (PT)
Occupational Therapist (OT)
Physiatrist (Physical Medicine and Rehabilitation)
Psychologist
A psychologist provides evidence-based treatments to individuals with low mood, anxiety and other psychological challenges after SCI. Changes in sleep, chronic pain, mobility, accessibility and life roles are carefully considered in regards to their impact on psychological function. If there has been a change in thinking, memory and behaviour in addition to having a spinal cord injury the psychologist can help with assessing and treating these challenges together with the family and other team members.
Spine Surgeon
Recreation Therapist
Vocational Rehabilitation
Outpatient/Spine Program Nurse
Assistive Technology
Clinical Dietitian
Peer Support
It can be pretty isolating feeling like you are the only person who understands your experience. Connect with people who have been where you are, through Spinal Cord Injury BC’s Living With Incomplete SCI Facebook group, or through our monthly live videoconference peer support for Ambulatory SCI peers. Contact info@sci-bc.ca for more information.
CONCLUSION
Conus and cauda equina injuries are more variable and less well understood, and rehabilitation can take longer. People with these injuries may struggle to understand their pattern of symptoms and establish routines to manage the bowel, bladder and sexual dysfunction that are common outcomes of these injuries. People living with conus or cauda equina injuries should work with their healthcare providers to understand how their injury affects their body and everyday life, and work to maximize their mobility and function through neurorehabilitation.
RESOURCES
Related Health Resources
- Cauda Equina Info Sheet – Queensland, Australia Spinal Injuries Unit.
- Bladder Management – Chapter in this resource, LivingWithSCI.ca, by Spinal Cord Injury BC and GF Strong Rehab Centre clinicians
- Bowel Management – Chapter in this resource, LivingWithSCI.ca, by Spinal Cord Injury BC and GF Strong Rehab Centre clinicians
- SCI Sexual Health.ca – Online SCI-focused Sexual Health resource authored by Vancouver Coastal Health/GF Strong Rehab Centre’s Sexual Health Rehab Team and Spinal Cord Injury BC
Peer Support:
- Living With Incomplete SCI – Private Facebook community group run by Spinal Cord Injury BC
This website contains general information about medical conditions and treatments. All information, content, and material of this website is for informational purposes only and are not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider. (c) 2024 Spinal Cord Injury BC
