PAIN
Pain is a part of life and an important adaptation to danger. The majority of people who have a Spinal Cord Injury (SCI) often experience pain, especially chronic pain. If you have pain after SCI, you are not alone. We know that pain can be complex and is a very individual experience, and it’s important to understand your pain and what influences it in order to better manage it.
- Introduction
- What is Pain?
- Why do we have pain?
- What Do I Need to Know?
- Acute vs. Chronic Pain
- Types of Pain After SCI
- Neuroplasticity
- What Can I Do?
- Understanding pain
- Changing our experience of pain
- Strategies for managing chronic pain
- Who Can I Talk to About This?
- Conclusion & Resources
INTRODUCTION
What is pain?
“An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described by the patient in terms of such damage” International Association for the Study of Pain (IASP)
Pain is a sensation produced by the brain in response to an outside sensation that could injure the body.
Normally, pain alerts you of danger to your body often before you are injured or injured badly. Pain triggers your body to make a move to protect yourself (such as pulling your hand away from a hot stove), or to think and behave differently (to warn you of injury to avoid making it worse) making it vital for healing.
With short term (acute) pain, there is usually a good reason, like when you need to protect a body tissue from future or further injury.
Why do we have pain?
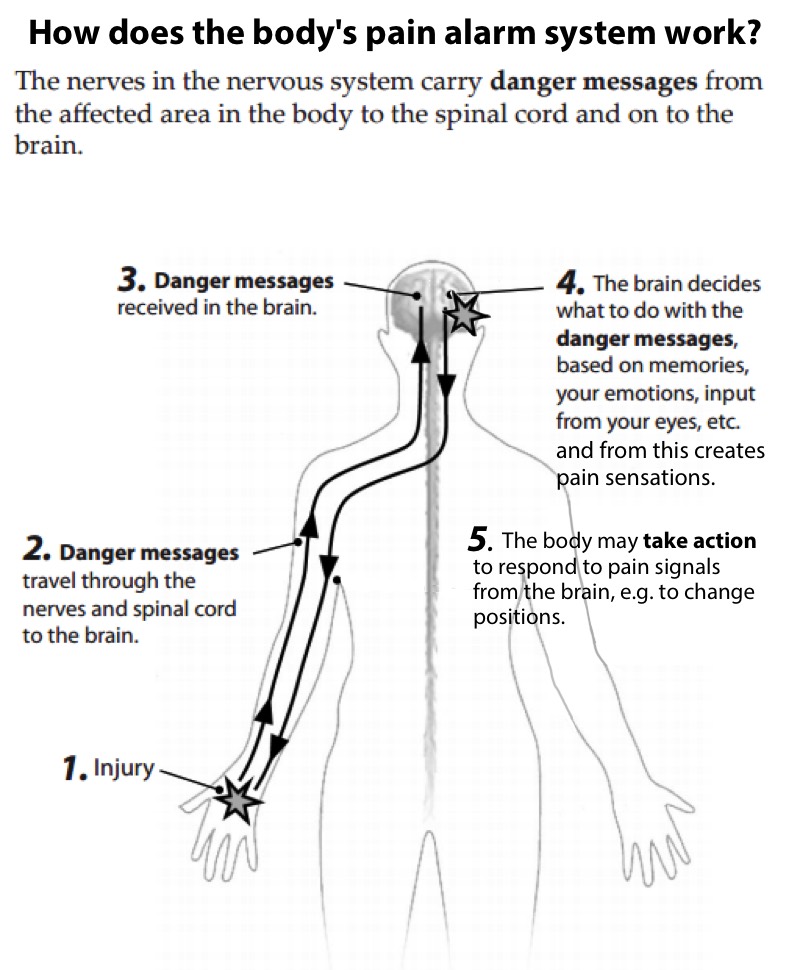
Pain acts as a warning to potential danger: Think of it as an alarm system, or as a pain alarm system. The pain alarm system is made up of the nervous system (includes the brain, spinal cord, nerves and sensory receptors), as well as the immune and hormonal systems.
The brain will decide if there is pain based on a variety of information:
- Past experiences/memories
- Feelings/mood/emotions
- Trust/feelings of safety
- The degree of threat to you that your brain perceives
Pain is made in the brain and signals us to take action to respond to the pain.
IF A danger or perceived danger to the body exists, AND action is required THEN the brain produces pain.
For example, when your brain receives signals from your senses that a limb is overstretched; and if it perceives that experience as a threat; you will feel pain. If it perceives an experience as non-threatening you will not feel pain.
Chronic pain
With chronic pain (pain lasting longer than three months), its purpose isn’t always obvious, and it may serve no useful purpose at all. Usually by three months any short term injury or painful stimulus has long passed or healed, but with chronic pain, you may still feel pain even thought there’s no imminent danger or action needed to protect the body.
We know that chronic pain exists long after the injury or danger has passed because the nervous system has become sensitized to pain. It may sense normally non-painful sensations and respond as if they were painful. Chronic pain is complex and is treated differently than acute pain, often with a focus on reducing the many triggers that sensitize the nervous system.
DID YOU KNOW?
Pain is made in the brain and signals us to take action to respond to it.
WHAT DO I NEED TO KNOW?
What we have learned in recent research
- Understanding how pain works is one of the best tools to help you manage your pain.
- With chronic pain, the amount of pain experienced is not always a good indication of what is happening in your body.
- It IS possible to change your experience of pain.
The more you understand about how pain works, the better you will be able to manage your pain.
What are the different types of pain?
- Acute Pain:
- Is a warning sign – a natural protection mechanism so you take notice before there is too much damage so you can take action (eg. burn, sprained joint, post-surgery).
- Main goal is protection.
- Intensity decreases with time and treatment as the tissues heal.
- Goes away once healing has happened.
- Chronic (persistent) Pain:
- Pain that lasts after the tissues have healed (longer than 3 – 6 months), when the problem is no longer an issue of current physical damage to your body.
- The pain alarm system becomes too sensitized & over responsive, just like a car alarm system that goes off whenever someone walks by. The alarm system is no longer useful.
- Treating pain like this involves many tools including medications, physical and other approaches that involve both mind and body together.
Pain doesn’t always equal tissue damage
It can be frustrating when pain continues despite treatments like medications. The good news is that your actions and behaviour can have a strong influence on your experience of pain.
When a Health Care Provider sees somebody who has pain, it’s very important for them to distinguish whether the pain is acute or chronic. The type of treatment that is recommended will depend on exactly what sort of pain is going on.
WHAT’S DIFFERENT NOW?
Pain after Spinal Cord Injury
After SCI, it is important to understand that pain can behave in different ways than before your injury, as the pathways that carry sensation have been damaged. Your body will use what is av ailable/left for it to carry the pain/danger signal to your brain. It is useful to learn about the different types of pain, as the treatment will vary depending on the type of pain you are experiencing. Pain after spinal cord injury (SCI) falls into one of three categories.
- Musculoskeletal (Mechanical) pain
- Produced when there is injury/damage to bones, muscles, tendons, joints and ligaments, e.g. inflammation following a strain or dislocation.
- Felt most often in areas where sensation is normal, however this is not always the case after SCI. For example, if you get a fracture or sprain in an area below the level of your injury the body may respond in different ways, such as with increased spasticity. Since you may not feel these injuries that occur below the level of your SCI they may go untreated for some time, which can lead to several problems.
- Affected (worsened or improved) by certain positions or activities.
- Visceral Pain
- Produced by signals of potential damage or inflammation from internal organs such as the stomach, bowel or bladder.
- Constipation or a full bladder may cause this type of pain sensation.
- Neuropathic pain
- Often occurs after damage or injury to the nerves.
- Caused by injured nerves are trying to reconnect that they fire and backfire, they can become over excitable and send inaccurate or distorted messages to the brain.
- Often described as tingling, numbness, throbbing, burning, stabbing, cold sensations, or a tightness. It can also make normally non-painful sensations (cold, clothing, or vibrations, etc.) feel painful even though there is no injury.
- Often occurs in areas where there is loss of some or all sensation, or around the border between sensation and lack of sensation.
- This pain is not typically influenced by movement or position, and can be felt as spontaneous bursts of pain.
- No tissue is actually being damaged/injured.
Neuroplasticity: how the brain and nervous system change
- Neuroplasticity is the scientific name for our brain and the nervous system’s amazing ability to change and adapt.
- Neuroplasticity happens when your brain and nervous system change by making new neural connections.
- If you practice a new skill many times, new neural connections in your brain will form, and you’ll get better at whatever skill you practice. That is helpful neuroplasticity.
- Neuroplasticity may be the process at the origin of chronic pain. Chronic pain happens when your nerves become super sensitized. They send pain signals over and over again to the brain, even when there’s no tissue damage. In this case, this is an unhelpful change in the nervous system, and appropriate treatments will aim to rewire the nervous system to make it less sensitized, thereby decreasing pain.
DID YOU KNOW?
Understanding neuropathic pain may reassure you that there is no new or ongoing damage to your body
WHAT’S MY ROLE?
Can we change our experience of pain?
Yes! There is hope. Pain comes from the brain’s reaction to signs of danger, but in chronic pain, responses depend on both physical and emotional components. There is both a physical and emotional part to pain. When we feel pain, many parts of our brain are active – especially the parts that control our thoughts and emotions. Our thoughts and emotions, both positive and negative, affect our nervous system.
The body can either amplify (turn up) excitatory signals, or block (turn down) the excitatory chemicals with calming signals from both physical and emotional pain experiences:*

Excitatory (“danger”) signals that increase our pain can come from fear, anger, negative thoughts and attitudes, depression, stress, and painful memories.
Calming signals that can decrease our pain can come from pleasant experiences, feeling safe, imagery, meditation and movement, or getting enough sleep. So the way you relate to your pain may help reduce how your nervous system is sensitized to pain.
Chronic pain is less about damaged tissue, and more about the sensitivity of our nervous system and how the brain is interpreting the information. A helpful way to live with chronic pain is to learn how to turn down the sensitivity of your nervous system.
*Adapted from The Science of Pain. Handout, Hamilton Health Sciences Centre, Michael DeGroote Pain Clinic.
Tools for managing pain after SCI
There are many different ways to treat and manage pain. The main goal of pain management is to turn down the volume, or to desensitize and soothe the pain system. Each of these skills and tools can help turn down the volume of the pain & has a different target. Trying a few different methods together often gives the best results
Medication
There are many medications available that treat different types of pain, but they should be prescribed by a doctor who understands your condition, with the goal of improving your function or mobility. You may need more of some medications at first, but be able to taper down the dosage over time.
- Always take pain medicines as directed, and watch closely for side effects. Understand your meds and why they are prescribed to you.
- Different approaches can be used for different types of pain, whether neuropathic, musculoskeletal (bone/joint) or visceral. Medications work best when chosen and prescribed for the type of pain you are dealing with.
- Common medications for pain include analgesics like acetaminophen, non-steroidal anti-inflammatories (NSAIDS) like ibuprofen, opioids like hydromorphone, or anti-epileptics like Lyrica or Gabapentin.
Physical Approaches
- Breathing & meditation techniques can distract, relax, and change how the brain perceives and produces painful signals, for example paced/meditative style breathing techniques (2:4 2:4)
- Progressive relaxation
Movement-based Approaches
A regular and appropriate exercise program can help the body’s natural pain control system to kick in (i.e. swimming, cycling, wheeling). Regular exercise can also protect and preserve current mobility, such as learning about shoulder protection, seating, posture or positioning strategies.
Movement based therapies include physiotherapy (PT) occupational therapy (OT), Tai-chi, Yoga therapy, restorative yoga, or even breathing exercises like those used in yoga or meditation.
Mind and Body Approaches
Maintaining an active life
- Distraction & enjoyment (music, sports, movies, games, arts…)
- Meaningful activities, ie work, volunteering, hobbies.
- Sense of humor, laughter
- Learning to balance sleep, activity and energy
Mindfulness/Meditation
- Visualization/imagery (visualize your safe place)
- Relaxation techniques
- Reframe situation.
- Mindfulness/centering practices for stress management.
Emotional Support
Talking about your pain with a trusted friend, someone who also has SCI, or a professional counsellor can be very helpful. Talk therapy or psychosocial counselling from a psychologist or social worker can be helpful for coping with stress related to chronic pain, and can help you learn practical strategies to improve emotional and physical well-being, including pain management. (For more, check out Coping and Adjustment after SCI). It can also be very helpful to seek out someone who has experienced SCI pain before to hear how it was for them and how they manage it.
Just hearing that you’re not alone with the pain you experience can help reduce the stress of chronic pain. Looking to talk to someone who’s been where you are? Get in touch with Spinal Cord Injury BC.
RESOURCE
Here’s a more complete list of the types of medications for pain after SCI.
RESOURCE
Check out this great handout on chronic pain management strategies from Spinal Cord Essentials.
READ MORE
Canadian clinical guidelines for SCI neuropathic pain from The Spin.
READ MORE
Peer discussion of cannabis use for neuropathic pain from The Spin.
WHO CAN HELP ME?
It’s important to find and work with a team of clinicians (e.g. Doctor, Psychologist, PT, OT) and learn to understand how they help you manage your pain. Working actively with a team of healthcare providers can help you identify and respond to the many different factors that contribute to your pain and how it affects your life.
Some clinicians most commonly involved in helping you manage your pain include:
- Rehabilitation Medicine Doctor (Physiatrist)
- Family Physician (also known as a General Practitioner or Primary Care Physician)
- Anesthesiologist/Pain Specialist
- Psychologist or counsellor
- Physiotherapist
- Occupational Therapist
CONCLUSION
Take charge of your pain
- Never ignore a new pain, get it checked first.
- Learn about your pain & be curious about it: what type of pain are you experiencing? What are its triggers? What helps relieve it?
- Explore the different tools to help manage your pain, and don’t be afraid to try tools to address different triggers.
- Harm vs Hurt: know the difference. Not every hurt (pain) means harm (injury)!
- Pace yourself and your activities: understand the role of a balanced lifestyle.
- Have a plan for how to manage your pain, including what to do in case of a flare up.
- Whether or not your pain will go away, learn what factors help you reduce it. Let your pain become less mysterious!
- Be patient and persistent.
RESOURCES
Organizations and Support
PainBC – a BC-based partnership of clinicians, researchers and patients to educate, support and reduce the burden of pain.
Books
Explain Pain – David Butler and Lorimer Moseley (book)
Effortless Pain Relief: A Guide to Self-Healing From Chronic Pain – Ingrid Bacci, phD
Videos
Understanding Spinal Cord Injury Pain – Pain Management Network (AUS)
Collection of Videos exploring Spinal Cord Injury Pain – Pain Management Network (AUS)
Tools & Skills
Physical Activity Guidelines – Guidelines and tools for Adults with Spinal Cord Injury
Peer Support
Pain After Spinal Cord Injury – SCI BC Virtual Peer Session [Video]
Mindfulness and Living with Spinal Cord Injury – SCI BC Virtual Peer Sessions [Video]
Research
Pain Relief – Purdue University researcher Dr. Riyi Shi, The Spin (Spring 2014)
HARM VS HURT:
Not every hurt (pain) means harm (injury)! Understanding your pain can help you manage it.
READ MORE
Self-management techniques for pain and online tool Live Plan Be from The Spin.
This website contains general information about medical conditions and treatments. All information, content, and material of this website is for informational purposes only and are not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider. (c) 2024 Spinal Cord Injury BC