SKIN HEALTH
After a Spinal Cord Injury, there are specific risks for your skin that can dramatically affect health and mobility, but are preventable with the right knowledge and equipment. In this section, you will learn how a spinal cord injury (SCI) changes your skin, how to protect and care for your skin post-injury, and ways to prevent the most common risks and concerns. You’ll learn how to prevent pressure injuries, how to troubleshoot if problems do arise, and where to get help when you need it.
- Introduction
- What does skin do?
- How does skin change after SCI?
- What Do I Need to Know?
- Pressure injuries: definition and stages
- Pressure Injuries: causes and risk factors
- What Can I Do?
- Preventing pressure injuries
- Self Management and Problem Solving
- What to do if you have a pressure injury
- Who Can I Talk to About This?
- Conclusion & Resources
INTRODUCTION
 Human skin is not just a barrier between the body’s vulnerable interior and the outside world – it also aids in maintaining water balance and prevents invasion of bacteria. Skin has two main layers: the epidermis, closer to the outside, and the dermis, the thicker layer that is underneath it. These two layers are separated by the basement membrane, a layer of fibres that controls the release of cells that aid in the growth and healing of the skin and surrounding tissues. Skin is also a membrane from which information about the outside world is sensed, such as temperature, movement, texture. Within the skin’s layers are millions of sensory nerve cells that communicate signals from the surface to nerve fibres to the spinal cord and then to the brain.
Human skin is not just a barrier between the body’s vulnerable interior and the outside world – it also aids in maintaining water balance and prevents invasion of bacteria. Skin has two main layers: the epidermis, closer to the outside, and the dermis, the thicker layer that is underneath it. These two layers are separated by the basement membrane, a layer of fibres that controls the release of cells that aid in the growth and healing of the skin and surrounding tissues. Skin is also a membrane from which information about the outside world is sensed, such as temperature, movement, texture. Within the skin’s layers are millions of sensory nerve cells that communicate signals from the surface to nerve fibres to the spinal cord and then to the brain.
After an injury to the spinal cord, the nerves that communicate the sensations of pressure and discomfort and make us aware of the need to change position may no longer work or be as reliable as they were before injury. These nerves are unable to accurately alert you to imminent injury like a scald from hot water or skin pinched by a seatbelt. After SCI, the loss of this important information from the skin’s surface means that your body is no longer able to subconsciously protect itself from injury, so using conscious awareness becomes a new everyday task in order to protect your skin.
After SCI, your skin changes in several other important ways that may not be obvious at first.
- Skin itself changes, changing colour and temperature. The loss of nerve connection from the skin to the nervous system below the injury disrupts thousands of tiny fibres in the skin that control how the skin responds to stimuli. Both skin and nails become thinner, more brittle and can be more vulnerable to dryness and injury.
- Circulation of blood and lymph changes affect your skin after SCI: Without the squeeze of muscles in the calf and thigh against the veins in your legs, blood and lymph pool and only sluggishly return back to the chest area, leading to fluid collection in the legs and feet. Compression stockings are often used in hospital to reduce swelling and risk of deep vein thrombosis (DVT), but can also be worn regularly at home to help leg circulation and reduce swelling.
- Slowed circulation also contributes to slower wound healing below the injury level, and can also lead to fluid collection in the legs and feet, by slowing the flow of wound healing cells and building blocks to wound sites and delaying the removal of fluid and byproducts of healing from the wound.
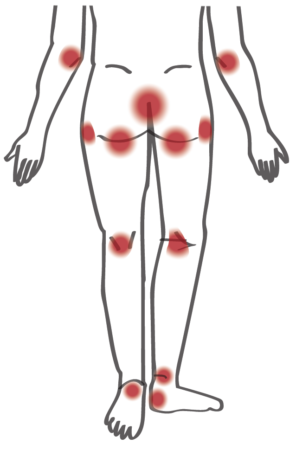
These changes after injury mean that living with SCI puts your skin at high risk for developing a pressure injury, which are injuries to the skin and the tissue that lies beneath the skin. Pressure injuries commonly develop on areas of skin that cover a bony area – such as the tailbone, sit bones, hips, or heels. Pressure injuries can also occur in places where the skin folds over on itself, such as the folds of the groin. They can start very small, but can quickly turn into a serious problem which may require a person to be on bed rest for weeks or even months while it heals.
WHAT DO I NEED TO KNOW?
Stages of Pressure Injuries
There are four stages of pressure injuries that range from reddening of the skin (Stage I) to deep wounds that go through all layers of the tissue down to the bone (Stage IV). They can be very hard to treat and very slow to heal. Sometimes, the injury starts under your skin and you can’t see it right away. These are called deep tissue injuries, and once they present themselves, they often show up as a dark red/purple colour. It’s important to take any discolouration of the skin seriously, and try to prevent it from getting worse.
Main Causes of Pressure Injuries
- Pressure: Lying or sitting still for too long reduces the blood supply to the skin and tissues under the skin, as they become “pinched” between the bone and the sitting/lying surface.
- . Pressure can also be a result of inadequate sitting or sleeping surfaces, tight clothing, seams, or buttons.
- Friction: Skin can get damaged by dragging across different surfaces, such as during a sliding board/pivot transfer, or from the sling used during a ceiling lift transfer.
- Shearing: Skin can get damaged from the shearing of tissues against each other, such as from sliding down in bed or sliding forward in the wheelchair.
Other Risk Factors
These factors are well known to increase the risk of developing a pressure injury, or to delay wound healing. This is not an exhaustive list, but are some of the most common contributors:
- Moisture/Dampness: The skin becomes fragile and more prone to skin breakdown when moist – such as from sweat, urine, or stool. It is important to keep the skin free from moisture as much as possible.
- Sensory Loss: Sensory changes or sensory loss below the level of injury are very common after SCI. This results in our body not receiving the signal that it is time to change position or that we are in a position that is causing discomfort to our skin and tissues.
- Poor nutrition/hydration: A poor diet that is low in vitamins and protein can make skin more likely to be damaged and delay healing. Your skin, like other organs in your body, also needs proper hydration to stay healthy, so drinking enough water is crucial.
- Smoking: Smoking decreases the blood flow to the skin, which makes it more fragile and can also delay healing.
DID YOU KNOW?
People with SCI have a 50-80% chance of having a pressure injury in their lifetime.
RESOURCE
Pressure Ulcers: Consumer Guide
WHAT CAN I DO?
Studies have shown that people with spinal cord injuries have a 50-80% chance of having a pressure injury in their lifetime. It is much easier to prevent a pressure injury than to heal a pressure injury, so every person with SCI should know and practice these prevention strategies every day.
Check your skin twice every day
 Check your whole body when you wake up (after lying down all night) and when you go to bed (after being in your wheelchair) – be sure to look for areas of redness/discolouration, blisters, or open areas.
Check your whole body when you wake up (after lying down all night) and when you go to bed (after being in your wheelchair) – be sure to look for areas of redness/discolouration, blisters, or open areas.- A red spot that does not go away after removing the cause of pressure (~15-20 minutes) is a pressure injury! Catching it at this stage is crucial so that you can find the cause and make changes to prevent it from getting worse.
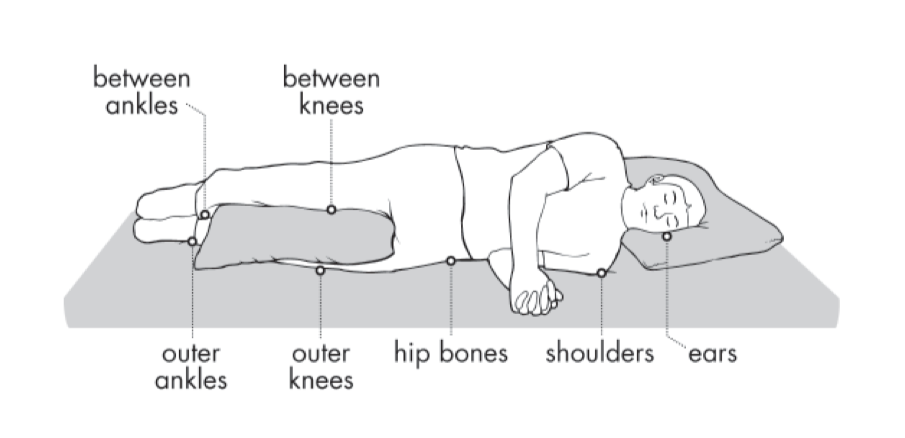
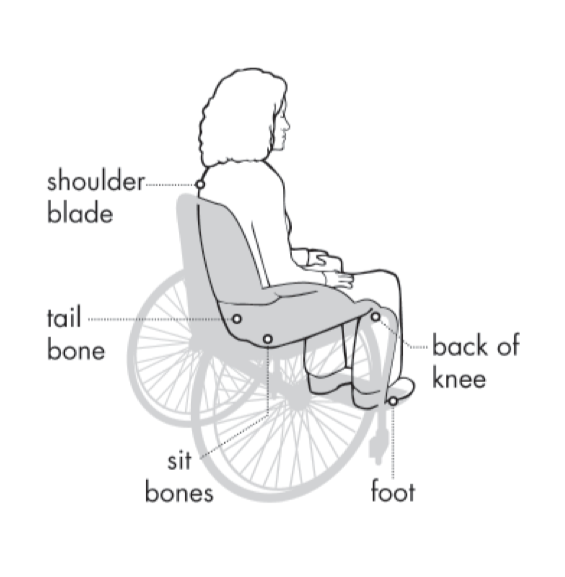
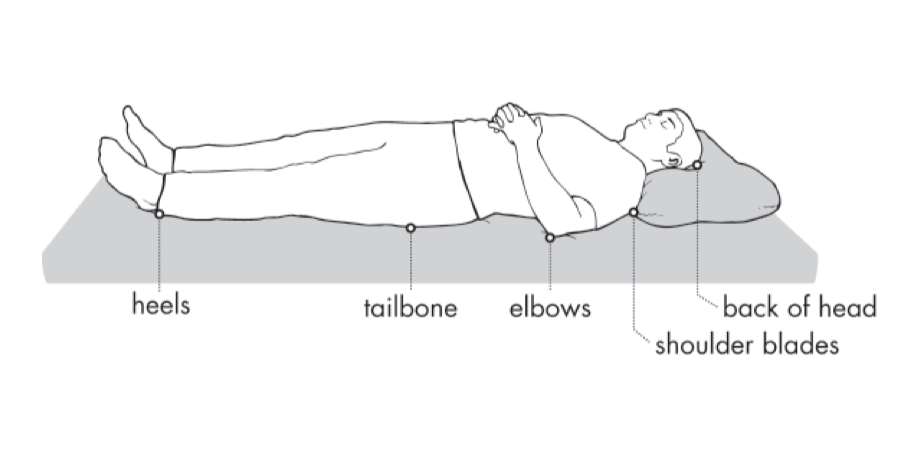
- Always check bony areas (back, elbows, tailbone, sit-bones, knees, heels). You can use a mirror to check yourself, if you are able to. If you can’t check yourself, learn to direct others (i.e. a caregiver) to check for you.
Shift your weight
- Weight shift every 15 minutes for 30 seconds to 1 minute.
- If you are in a manual chair, lean forward onto your elbows, or lean to the side to shift your weight.
- If you are in a power chair, tilt your chair 45- 60 degrees (almost lying down).
- In bed, find out how many turns you need each night to keep your skin healthy.
Ensure proper surfaces
Work with your health care professionals, such as your OT and PT, to ensure your surfaces (cushion, mattress, backrest) are right for you, and that they are adequate to relieve and distribute pressure and prevent pressure injuries.
Transfer safely
Ensure you have enough clearance during transfer – don’t drag yourself across surfaces (such as the wheel of manual chair). If you use an overhead lift, ensure your sling is placed properly in order to prevent friction or shearing.
Keep your skin clean and dry

Read about Foot Care from Bonnie Venables Nybo, GF Strong Rehabilitation Centre’s SCI Outpatient Nurse
- Bowel and bladder accidents can cause skin problems. Try to stick to your bladder and bowel routine to prevent having accidents.
- If you are having bowel and bladder problems that you are not able to manage, be sure to seek help from health care providers.
- If exercising, make sure to change out of sweaty clothes and clean your skin.
- Remember your feet! Care for your skin includes your feet and toenails!
Take care of your equipment
- Check your cushion every day – if it’s an air cushion – is the inflation correct? Is it on your chair the right way?
- Make sure all your equipment is working and in good shape.
- Every 3-5 years have an occupational therapist or physiotherapist check the fit of your equipment. If you don’t have an OT or PT, ask your family physician for a referral to GF Strong’s outpatient spinal cord program or the local health unit to access these services.
Eat a proper diet and drink plenty of water
- Eat a healthy diet following Canada’s Food Guide and ensure you maintain a healthy weight.
- Drink water to keep well hydrated. Dark urine or a low amount of urine are signs of dehydration.
- For more information on eating well, contact a dietician in BC through HealthLinkBC’s 811 hotline.
Pressure Injury Trouble Spots: The photos below show common areas that are at risk for pressure injury, both sitting in a wheelchair and in bed. Make sure to check these areas during your skin checks every day, and take action when you see any red spots particularly in these areas.
IMPORTANT!
A red spot that does not go away after removing the cause of pressure is a pressure injury!
SELF MANAGEMENT AND PROBLEM SOLVING
What to do if you find a trouble spot or pressure injury
If during a skin check, you or your caregivers find a red area, blister or open skin, the first step is to remove pressure from that spot right away – or get off of that spot. You need to stay off of the area until you and your team determine the cause. For example, if it’s on your tailbone, alternate between lying on your left and right sides when in bed to offload pressure from that area.
Next, you need to problem solve the cause of the pressure injury, and treat the cause. Problem-solving is a useful way to deal with situations when you’re not sure what to do. See below for a handy 5-step method for solving problems you encounter with your skin – there’s also a PDF resource of the steps as well!
Step 1 — Identify the problem: Start by getting a clear picture of what’s wrong. Before you jump to conclusions, take the time to investigate – where is the redness located? What is the shape or pattern of the redness? Inspect your skin thoroughly and pay special attention to areas you might normally overlook.
Step 2 — Find the cause: Once again, you want to be thorough; here are some questions to consider (remember, this is not an exhaustive list, just a place to help start your problem solving):
- Were you sitting or lying in one position too long?
- Was it in your bed? In your wheelchair? On your commode? In your car?
- Is there enough air in your cushion? Was your cushion on backwards?
- Did you do a bad transfer?
- Are you having more spasms/spasticity?
- Are your clothes or your shoes too tight?
- Was there anything new in your routine, such as a new surface or activity?
Step 3 — Brainstorm solutions: Using the information you have, think of a number of possible solutions. You may be able to address the problem yourself and prevent the situation from getting worse. The solution will depend on the location and the cause of the wound.
- Pressure: Remove sources of pressure, offload the area.
- Shearing/Friction: Check your transfers, sling placement, limit raising the head of the bed.
- Moisture: What’s causing the excess moisture? Make sure you’re sticking to your bladder and bowel routine and are on the right surfaces if moisture is an ongoing issue.
Step 4 — Try one and evaluate results: Try one of the solutions you or your health care professional identified, starting with the one that seems likely the most likely solution. If it works…great! Just make sure to follow-up and ensure that the problem is truly solved. If it doesn’t work, try another solution. You may need to repeat this step several times.
Step 5 — Know when to ask for help: Don’t try to take everything on by yourself. When it comes to something as important as your skin, it’s better to be safe than sorry, so when in doubt, ask for help. You should be able to recognize the signs of a serious pressure injury that requires medical attention. In some cases, the only solution may be to get help. Talk to a health professional to learn how to manage your wound and problem solve any equipment or equipment changes that may have to occur.
RESOURCE
Troubleshooting Pressure Injuries
WHO CAN I TALK TO ABOUT THIS?
Occupational Therapist
Occupational Therapists (OT) are essential for troubleshooting pressure ulcers and finding equipment that protects your skin from pressure injuries, especially in high risk areas. You will see an OT while you are in acute rehabilitation at GF Strong and other rehab hospitals, and you can access seating and OT through GF Strong’s Spinal Cord Outpatient Program. If you can’t get to GF Strong, you can ask your Family Physician for a referral to community health OT services which may be available through your local Health Authority in BC.
Family Physician
Wound Clinic
CONCLUSION
The key to maintaining healthy skin is to develop an understanding of why your skin is more at risk after SCI and to have a mindset of prevention. Pressure injuries can take a very long time to heal and can disrupt your everyday routines and activities. Prevention is extremely important, so make sure you’re completing frequent weight shifts and ensuring you have the proper equipment, as well as completing daily skin checks to watch for new areas of redness. When in doubt, get a health professional involved, such as your family physician, a wound care nurse, or an occupational therapist to help you with problem solving.
SUMMARY OF RESOURCES
- Pressure Ulcers – a Consumer Guide – Consortium for Spinal Cord Medicine/Paralyzed Veterans of America (PDF)
- Maintaining Healthy Skin – Northwest Regional SCI Centre, University of Washington (PDF)
- Preventing and Treating Pressure Ulcers Guide – Spinal Cord Injury Ontario and Ontario Neurotrauma Foundation (PDF)
- Skin Health – SCIRE Community (web page)
- Pressure Sore Prevention – Spinal Cord Essentials (PDF)
- Pressure Relief Techniques – Spinal Cord Essentials (PDF)
Video Content:
- Skin – SCI-U (website/video)
- How to Prevent Pressure Injuries When You Use a Wheelchair – Craig Hospital (video)
This website contains general information about medical conditions and treatments. All information, content, and material of this website is for informational purposes only and are not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider. (c) 2024 Spinal Cord Injury BC

